By guest author: Anne Anthony
Has this ever happened to you? You had a full day of clinic appointments performing a variety of professional services for patients. The claims for these appointments were filed and processed, and the remittances or explanations of benefits from the insurance plan stated that some of the services performed were denied “due to NCCI edits”. What does that mean?
NCCI stands for the National Correct Coding Initiative (NCCI or CCI), which was implemented by the Centers of Medicare and Medicaid Services (CMS) to promote national correct coding methodologies and to control improper coding leading to inappropriate payments for Part B provider claims. When certain codes are submitted together on a single claim, the NCCI code pair edits (known as the Procedure-to-Procedure or PTP code pair edits) are automatically applied during claims processing to prevent improper payment for incorrect code combinations. While certain CPT (Current Procedural Terminology) codes are very specific in the description of a single service, others may describe a procedure that consists of many services. Because these code descriptors may not list every service included in a specific procedure, providers may be unsure when services are considered inherent to the primary, more comprehensive procedure performed during the patient encounter.
CMS publishes tools to help providers avoid coding and billing errors and subsequent payment denials. Along with the NCCI manual, providers may also find the Medicare Learning Network booklet helpful on how to use these tools. The NCCI tables and PTP code pair edits are updated quarterly. These updates help identify services that may be considered a component of the more comprehensive primary service; those that may be mutually exclusive of each other and unlikely to be performed at the same encounter, or those potentially separate and distinct services which may be payable if the use of a modifier is justified.
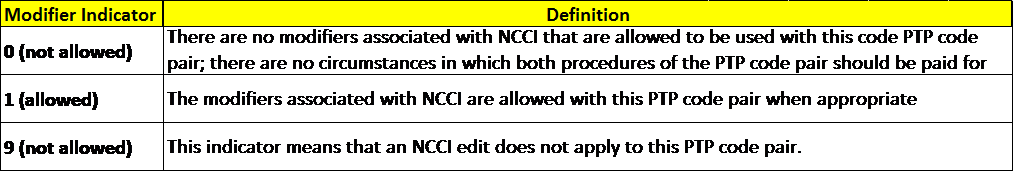
Now you may be asking, how do I know if a service is considered a component of another service I perform? The PTP code pairs are presented in the NCCI tables with CPT codes under columns labeled Column 1/Column 2 within the PTP code pair tables. When a code pair is submitted on a claim, the Column 1 code may be eligible for payment while the Column 2 code may be denied. In some scenarios, a provider may be eligible for payment of both codes if each service is considered clinically appropriate and an appropriate coding modifier is appended. Modifiers should only be appended if the clinical circumstances justify the use of the modifier and the patient’s medical record includes documentation to support the utilization. Never append modifiers to a CPT code to merely bypass a PTP code pair edit. Rather, indicate that a clinical rationale has been identified and documented. The PTP code pair tables also provide helpful guidance on the appropriate utilization of modifiers, including information on the potential applicability for the code pair, or lack thereof, in the form of a modifier indicator, as shown in the example below.
Below is a partial excerpt from the CMS NCCI Practitioner procedure edits table highlighting a few audiology service code pairs. The procedure listed in Column 1 represents a primary service performed, while the procedure in Column 2 represents the subsequent service(s). Whether or not a modifier may be applicable or allowed is shown by the indicator of 0, 1, or 9 in the far right column.
Understanding the nuances of reimbursement is only one aspect in building a sustainable practice. Cochlear offers support to providers to help navigate these areas. Please visit the Cochlear Reimbursement Solutions website to identify your Cochlear Regional Reimbursement Manager or call the Cochlear Coding Support Program at 1 800 587 6910 for additional information.
About our guest author:
Anne Anthony is one of three geographically-based hearing implant reimbursement experts available to assist you with coding, payment, payer coverage, contracting, and other reimbursement related challenges. Anne’s contact information, along with that of her colleagues and a more detailed description of the reimbursement support offered by Cochlear’s Regional Reimbursement team, can be found on the Reimbursement Support page of Cochlear’s US Professional Resources Website. Please do not hesitate to reach out to the Reimbursement Manager associated with your geography for reimbursement assistance or for questions related to this article. Cochlear offers coding assistance through the Coding Support Line accessible by calling 1-800-587-6910 between the hours of 8 AM – 3 PM Mountain time zone or via email at codingsupport@cochlear.com. For pre-surgical insurance support, OMS is available to assist with pre-authorizations and appeals and can be reached at 1-800-633-4667 option 4.