
By Amy Donaldson, Professional Education Manager, Cochlear Americas
Gagnon, Erika B., Eskridge, Hannah, Brown, Kevin D.
Pediatric cochlear implant wear time and early language development
Sep 29, 2019:1-6
Cochlear Implants Journal
In today’s busy clinical environment, clinicians who value research-based practice often struggle to keep up with current literature. To help, we’re excited to offer a new ProNews Blog monthly feature – Journal Club! Each month, rotating guest authors will present a current journal article summary.
This month’s Journal Club explores a recent study by the team at the University of North Carolina published in September 2019, Pediatric Cochlear Implant Wear Time and Early Language Development. This article may be especially useful for those clinics working with pediatric recipients as a resource for counseling on device use.
What did the study investigate?
This study was designed to examine the relationship between device wear time in pediatric recipients and their language development.
For children with hearing loss, consistent access to auditory information with either hearing aids or cochlear implants is associated with better speech and language development.1,2,3,4 Unfortunately, clinicians can’t always rely on parental report of device use – some studies have shown that they overestimate device use by an average of 2.6 hours per day.5
Modern cochlear implant systems now have datalogging available to help clinicians objectively track device use, but it can be unclear how these results should be interpreted or what is the impact of differences in wearing time. If a one-year-old uses their device seven hours per day, is that enough to provide access to spoken language? What about the same use per day for a five-year-old? This study attempted to answer these questions.
How did they do it?
The authors utilized datalogging in the Nucleus® sound processor and applied a measurement called “Hearing Hour Percentage” or HHP to track the amount of device use:
HHP = total wear time/median awake time * 100
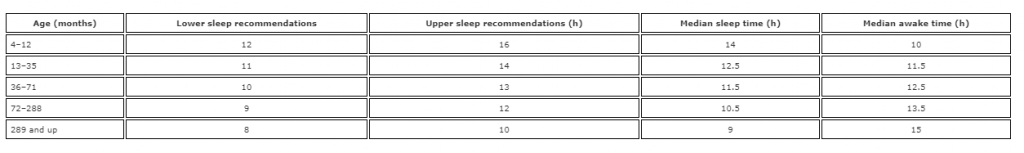
This measurement provides more information than just hours per day since it considers the waking hours of each day for children of different ages. For example, according to the American Academy of Sleep Medicine6 the average median awake time for a one-year-old is 11.5 hours; for a five-year-old, it’s 12.5 hours. That makes sense – younger children sleep more. So seven hours of device use for the one-year-old is 61% of their awake day; but for the five-year-old, it is only 56%. See table below:

Here are the key features of the study:
- 37 children implanted prior to age 5
- Average age of implantation: 1.97 years
- Followed for the first year of device use
- All using Nucleus 6 technology or later
- Language tests: The Preschool Language Scale: Fifth Edition (PLS-5) or Oral and Written Language Scales: Second Edition (OWLS-II)
Results
The study found HHP of the 37 children ranged from 18% to 117% with an average of 63%. More than half of the group achieved an HHP of over 60% by the end of their first year of device use. This is interesting since many professionals would recommend device use during “all waking hours” but this study demonstrated that average usage of cochlear implants in children may only be about 60% of waking hours.
The study found a positive correlation between HHP and receptive language abilities – the more recipients used their device, the better their receptive language – although the correlation was not significant for expressive language abilities. This may have been because they only followed the children for one year after device use and expressive language development lags behind receptive language development. Device use accounted for 40% of the variability in receptive language for the children confirming that while device use is important, it is still only one variable in outcomes for children.
Discussion
The results of this study support the importance of consistent device use for language development in children and highlight device datalogging as a critical tool in measuring progress. The findings may also encourage professionals to consider how they counsel parents of young children who are using cochlear implants. Combining datalogging with information about average awake time allows clinicians to determine the HHP for an individual child. Counseling a parent to have their child use the device “all waking hours” may be helpful, but it might be even more useful to encourage use for a percentage of the child’s awake time and measure their progress by increasing that percentage.
Pediatric clinicians encourage families to achieve “full time” device use. This study helps define what that number should look like for children of different ages and gives parents and caregivers specific goals. While datalogging can help clinicians track progress during clinic visits, Hearing Tracker is now available for parents to use between visits. Hearing Tracker is available for the Nucleus 7 sound processor in the Nucleus Smart App, and is available in both iOS and Android™ devices.
With Hearing Tracker, datalogging and device use information is not just available to clinicians but can be seen real-time by parents and caregivers, supporting device use and helping to support language development in children who use cochlear implants.
Learn more about this exciting clinical strategy by accessing the publication here and stay tuned for next month’s edition of Journal Club!
About our guest author:
Amy Donaldson is an Audiologist and Professional Education Manager for Cochlear Americas. She received her Master’s Degree in Audiology from the State University of New York at Buffalo and her AuD from the University of Florida. She was privileged to begin her career as a pediatric audiologist and gain extensive clinical experience in implantable hearing devices at the University of Michigan in Ann Arbor and at the Manchester Cochlear Implant Programme in the United Kingdom. After working for several years as an Educational Audiologist and Technical Support Audiologist in the hearing aid industry, she returned to hearing implants and Cochlear in 2011.
References:
- Weisman KB, Warner-Czyz AD (2018) Inconsistent device use in pediatric cochlear implant users; Prevalence and risk factors. Cochlear Implants International, 19, 131-141.
- Toblin, JB, Harrison, M, Ambrose, S, Walker EA, Oleson, JJ, Moeller MP. (2015) Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36(Suppl 1):76S-91S.
- Easwar V, Sanfilippo J, Papsin, B, Gordon, K. (2018) Impact of consistency in daily device use on speech perception abilities in children with cochlear implants: datalogging evidence. Journal of the American Academy of Audiology, 29:835-846.
- Guerzoni L, Cuda D (2017) Speech processor datalogging helps in predicting early linguistic outcomes in implanted children. International Journal of Pediatric Otorhinolaryngology, 101:81-86.
- Walker EA, Spratford M, Moeller MP, Oleson J, Hua O, Roush P, Jacobs S. (2013) Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech & Hearing Services in the Schools, 44(1):73-88.
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA et al (2016) Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. Journal of Clinical Sleep Medicine, 12(6):785-786.
Android and Google Play are registered trademarks of Google Inc.
The Android robot is reproduced or modified from work created and shared by Google and used according to terms described in the Creative Commons 3.0 Attribution License.
The Cochlear Nucleus Smart App is available on App Store and Google Play. For complete smartphone compatibility information, please visit www.cochlear.com/compatibility.


