By Mary Beth O’Sullivan, Professional Education Manager, Cochlear Americas
Use of Neural Response Telemetry for Pediatric Cochlear Implants: Current Practice
Galit Almosnino, MD1 , Samantha Anne, MD2, and Seth R. Schwartz, MD, MPH1
Annals of Otology, Rhinology & Laryngology
2018, Vol. 127(6) 367–372
In today’s busy clinical environment, clinicians who value research-based practice often struggle to keep up with current literature. To help, we’re excited to offer a Cochlear ProNews monthly feature – Journal Club! Each month, rotating guest authors will present a current journal article summary.
This month’s Journal Club explores a 2018 study, Use of Neural Response Telemetry for Pediatric Cochlear Implants: Current Practice. Successful management of medical practices today requires the ability to prioritize both patient outcomes and clinic efficiency. Cochlear implant programs that work with young children and other special needs populations may feel this even more acutely due to time spent testing and additional unbillable time spent counseling families.
The availability of electrically evoked compound action potentials (ECAP) measurements as a clinical tool revolutionized pediatric cochlear implant management by providing objective responses to auditory stimuli. For example, neural response telemetry (NRT) is a version of ECAP. NRT data has become increasingly fast and easy to collect in the operating room (OR) with the development of remote management capability. Clinics may obtain this data to confirm function of electrodes and electrode placement in the OR, and this information is also helpful during the initial activation. Very young children may not respond to the traditional programming stimuli on the first day, leaving the clinician unsure where to set parameters and causing worry for the family regarding device function.
The authors noted highly variable use of ECAP tools across the country and took the initiative to work toward developing best practice guidelines by first establishing current practice across the country.
What did the study investigate?
The authors developed a 12-question survey that was sent to 110 cochlear implant clinic directors to investigate use and benefit of the ECAP tool.
Why is this important?
Establishing best practice guidelines is an ideal means of ensuring consistent and positive outcomes for patients. It is particularly important when working with medical devices in children and other vulnerable populations. The authors determined that the first step in developing best practice guidelines was to identify current practices across various regions and practice settings.
How did they do it?
Here is the need-to-know:
- Survey sent to 110 CI center directors
- 32 invited participants (29%) completed the survey
Results and Discussion1
- >80% reported that test time took less than 15 minutes
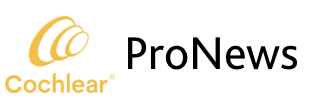
- 72% use intraoperative ECAP with pediatric patients
- >50% use this tool to confirm placement and to assist with post-operative programming
- 63% report improved ability to program at IA
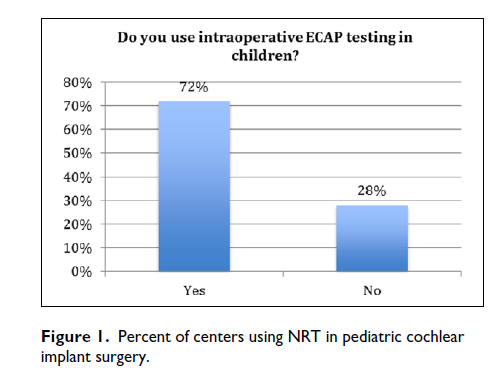
- 50% report that results improve satisfaction with initial activation
- <50% report results prompted different management during cochlear implantation
- 78% report testing occurred from a remote location
- 47% reported that data collected in the OR makes the initial activation more efficient, while 44% said it did not have any effect
Since the OR is a costly place to perform tests, any additional beneficial test results must be reliable, provide useful clinical information and also be fast and easy-to-use. The results also give the family information on what to expect at the initial activation, which is both reassuring and time-saving on a day that can be loaded with emotion. NRT uniquely uses the subtraction method to reduce stimulus artifact. The ability for clinics to collect data remotely adds to the efficiency and usability of the data collection as a tool.
Results suggest that the greatest benefit of NRT is for clinic efficiency post-operatively rather than as a primary tool for confirming device placement intraoperatively. Used in combination with imaging such as X-ray or CT scan will provide a higher confidence for that purpose. The authors recognize the limitations of a survey as a research tool, pointing out that additional data correlating the data to outcomes would be extremely useful. However, the survey strongly argues that the ability to quickly and easily start the initial activation with a viable map is a cost-saving benefit that also provides significant reassurance for the audiologist as well as the family.
Learn more by accessing the publication and stay tuned for next month’s edition of Journal Club!
About our guest author: Mary Beth O’Sullivan is a Professional Education Manager at Cochlear Americas, creating educational opportunities for cochlear implant professionals using research and best practice guidance. Mary Beth has been an audiologist for 20 years, working in clinical settings ranging from large university hospitals to private practice prior to dedicating herself to the education side of the field.
References
- Almosnino, G., Anne, S., Schwartz, S.A. (2018). Use of neural response telemetry for pediatric cochlear implants: current practice. Annals of Otology, Rhinology & Laryngology 127(6) 367-372.