By David Friedmann, MD, MSc
Cochlear Case Studies is a new series on Cochlear ProNews that highlights relevant clinical and surgical scenarios surrounding the latest hearing industry topics and research. We’re excited to partner with professionals to highlight their experiences surrounding specific patients. This first installment will specifically feature surgeons, their cases and contributing factors for use of different electrodes.
Case Study
Patient background
This patient is a middle-aged male with a long history of bilateral otosclerosis first diagnosed in his 20’s when he began wearing hearing aids. In otosclerosis, a bone disease which affects the otic capsule, both conductive hearing loss and sensorineural hearing loss can occur—especially as the disease progresses. Stapes middle ear surgery and hearing aids can address the conductive component of the hearing loss. With a profound mixed loss, it may be difficult to achieve the necessary level of amplification for adequate audibility with hearing aids alone. In such cases, stapes surgery may improve aidability with amplification. In cases where speech discrimination remains poor, a cochlear implant can be considered.
In this particular patient, he reported declining benefit from his bilateral hearing aids and had become more dependent on speech reading with minimal open set speech understanding with hearing aids. With no prior ear surgery, we discussed the role of stapes surgery for his profound mixed loss to improve his ability to wear hearing aids. Surgery was attempted on his worse hearing RIGHT ear which partially closed his air-bone gap and led to improved “aidability” with his hearing aids. This led to improvement in his aided word recognition score bringing it to 34%. We subsequently discussed his options for stapes surgery or a cochlear implant for his contralateral LEFT ear, but overall expectations were tempered given his advanced otosclerosis.
Candidate evaluation
Preoperative audiogram demonstrated bilateral profound loss (suspected mixed component in both ears) with normal tympanograms and unaided aided speech discrimination of 34% in RIGHT (ear with prior stapes surgery) and 0% in LEFT ear at 100 dB HL (MCL). Aided scores were 40% on RIGHT and 14% on LEFT. After thorough discussion with the patient about outcomes with otosclerosis, the decision was made to implant the LEFT ear with a cochlear implantation.
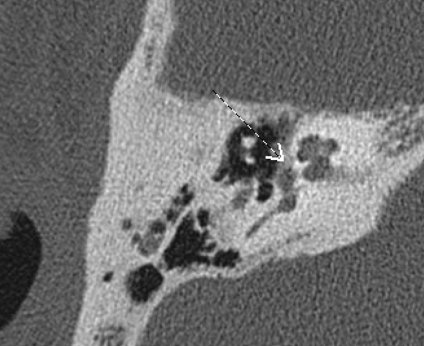
Electrode selection
Given concerns for cochlear otosclerosis, a Contour AdvanceTM (512) was used for two main reasons. The stiffness of the stylet provides the opportunity to insert in the setting of partial ossification or fibrosis. Additionally, based on our Center’s experience, perimodiolar electrodes are preferred in cases of cochlear otosclerosis as the array resides further from the lateral wall where spread of current can lead to facial nerve stimulation from the cochlear implant. This reduces the likelihood of the facial nerve being stimulated by the cochlear implant.
Surgical observation
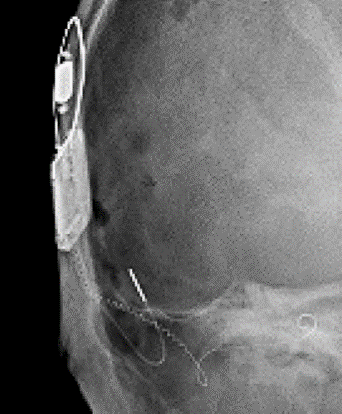
There was ossification at basal end which was easily removed revealing a patent lumen. Given this, the depth gauge was not necessary. The electrode array was inserted using the Advance Off-Stylet (AOS™) technique. A full insertion was achieved and confirmed with intraoperative X-ray. Neural response telemetry was completed.
How are things going for the patient?
At his one-year evaluation of the left cochlear implant surgery, this patient had an open set word score of than 94% in CI ear alone. There have been no issues with facial nerve stimulation. He continued to be bimodal (HA+CI) and deferred a sequential CI due to the pandemic. In October 2020, he went uncomplicated sequential RIGHT CI with a CI612. He is very happy with bilateral cochlear implants and performing well.
To hear more from Dr. Friedmann, listen to our Cochlear Case Studies surgeon panel webinar!

About the author:
David R Friedmann, MD, MSc is a neurotologist, cochlear implant surgeon and clinical investigator at NYU Grossman School of Medicine. His research interests include cochlear implants in unique populations including those with residual hearing, single-sided deafness and abnormal cochleae as well as cochlear implant electrode design. Dr. Friedmann is a nationally funded principal investigator studying the management of severe hearing loss.


