Co-authored by Kristen Caron, AuD
With recent expansions in cochlear implant (CI) candidacy—including Medicare’s updated criteria and the FDA’s approval for single-sided deafness and asymmetric hearing loss—the number of adults eligible for cochlear implantation is growing rapidly. As more patients become candidates, audiologists must adapt and innovate to meet this rising demand.
A national survey recently published in Ear & Hearing by Zwolan et al. (2025) offers a timely and comprehensive look at how audiologists across the United States are evolving their care delivery. Between November 2023 and January 2024, 209 audiologists who work with adult CI candidates and recipients completed a 48-question survey. Of these, 21 questions focused on pre- and post-operative care, appointment availability, scheduling practices, use of telehealth and strategies for triaging follow-up care. The primary aim was to explore how clinical procedures have evolved and to identify opportunities for improvement that could enhance access to CI services.
Trends in Access and Efficiency
More than half of respondents (51%) reported wait times of less than four weeks for a new adult CI evaluation—a positive indicator that clinics are finding ways to accommodate new patients more quickly. However, disparities emerged based on setting: audiologists in private practice reported significantly shorter wait times than those in academic or hospital-based environments.
For preoperative candidacy evaluations, 54% of clinicians reported completing the process over two appointments, with 82% spending two to three hours total per patient. Private practice audiologists spent significantly less time on these evaluations compared to their counterparts in academic and hospital settings. Additionally, 53% of respondents indicated they always or frequently involve CI manufacturers in preoperative counseling to enhance patient education. While manufacturer-based counseling did not have a significant effect on preoperative time spent with the patient or on wait times, this offering can enhance patient education and increase confidence and satisfaction.
Post-operative care is also evolving. The median number of follow-up appointments reported by survey participants in the first year after implantation was six, down from previous reports of seven to eight visits.1-4 The most common follow-up intervals were at one, three, six and twelve months. When considering appointment duration, device activation remains the longest, averaging just over 100 minutes, while subsequent visits typically last 81–84 minutes. As with pre-operative care, clinicians in private practice reported spending less time with patients post-operatively. Importantly, a 2023 study by Porps et al. found no evidence that reduced time with patients compromises hearing outcomes.3 This can give you confidence that following a reduced follow-up schedule will not compromise your patient care.
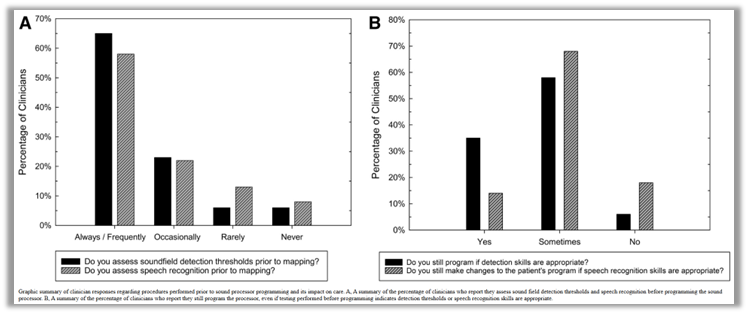
One dilemma clinicians often face is the optimal time to evaluate detection thresholds and speech recognition – should that occur prior to programming (when results could theoretically indicate that reprogramming is not necessary) or following readjustment of psychophysical levels? Many survey respondents indicated they reprogram CI devices, even when detection thresholds and speech recognition scores obtained prior to mapping are within expected ranges. This finding indicates there may be an opportunity to further develop standardized criteria for determining when reprogramming is needed, potentially reducing unnecessary appointments and improving both clinic efficiency and patient convenience.
The Role of Telehealth in Expanding Access
Only one-third of clinicians reported using telehealth in their CI programs, primarily for triage, troubleshooting, and preoperative counseling. Remote tools like Remote Check† have shown promising results, delivering outcomes comparable to in-person visits while saving clinician time.5 However, barriers such as clinic policies, reimbursement concerns, and patient comfort with technology continue to limit broader adoption.
Rethinking Annual Follow-Ups
Although 86% of clinicians recommend annual follow-up visits after the first year of CI use, real-world adherence is low. Shapiro et al. reported that only 29% of CI patients returned for the recommended 12-month visit, and just 22% returned at 24 months.1 This raises important questions about the necessity and format of annual visits, especially for patients who demonstrate stable performance. Telehealth tools that enable clinicians to remotely monitor patient performance, such as Remote Check, may offer an alternative that provides both patients and clinicians with assurance that maximal benefit is being achieved from the device without requiring an in-person visit. This allows for patient-centric monitoring and provides clinicians time to focus on meeting the needs of new patients or those with the highest clinical needs.
Moving Forward: A More Accessible Future
As CI candidacy expands, the audiology community is well-positioned to lead the way in reimagining care delivery. While only an estimated 11% of U.S. audiologists currently specialize in CI services, this growing demand presents an exciting opportunity to innovate. Rather than a limitation, this workforce gap can serve as a catalyst for progress—encouraging streamlined protocols, expanded training and greater integration of telehealth.
This study highlights the meaningful steps audiologists are already taking to meet the needs of a broader CI population. From reducing wait times and simplifying evaluations to optimizing follow-up schedules and exploring remote care options, the field is clearly moving toward a more accessible, efficient and patient-centered model. These shifts reflect more than operational improvements, they demonstrate a deep commitment to helping more people while still delivering timely, personalized care that supports each patient’s journey.
Looking ahead, continued innovation will be essential. By embracing milestone-based programming, leveraging remote assessment tools and advocating for supportive telehealth policies, clinics can ensure that more adults have access to the life-changing benefits of cochlear implantation, when and where they need it most.
To find out how Cochlear can help your clinic implement some of these changes, see a recently published ProNews article “Implementing Protocol Changes in your Clinic: How Cochlear Care Can Help.”
Read the full article: Zwolan, T. A., Holcomb, M., Buck, B., Adkins, W., Snapp, H., & Prentiss, S. (2025). A survey of current audiology practice in adult cochlear implant programs and its impact on access to care. Ear & Hearing.
- Shapiro S. B., Lipschitz N., Kemper N., Abdelrehim L., Hammer T., Wenstrup L., Breen J. T., Grisel J. J., Samy R. N. (2021). Real-world compliance with follow-up in 2,554 cochlear implant recipients: An analysis of the HERMES database. Otol Neurotol, 42, 47–50.
- Zwolan T. A., Presley R., Chenier L., Buck B. (2021). Investigation of an outcomes-driven, computer-assisted approach to CI fitting in newly implanted patients. Ear Hear, 42, 558–564.
- Porps S., Bennett D., Gilden J., Ravelo K., Buck B., Reinhart P., Hong R. (2023). Effects of an evidence-based model for cochlear implant aftercare delivery on clinical efficiency and patient outcomes. Cochlear Implants Int, 24, 325–334.
- Dunn C. C., Zwolan T. A., Balkany T. J., Strader H. L., Biever A., Gifford R. H., Hall M. W., Holcomb M. A., Hill H., King E. R., Larky J., Presley R., Reed M., Shapiro W. H., Sydlowski S. A., Wolfe J. (2024). A consensus to revise the minimum speech test battery-version 3. Am J Audiol, 33, 624–647.
- Carner M., Bianconi L., Fulco G., Confuorto G., Soloperto D., Molteni G., Sacchetto L. (2023). Personal experience with the remote check telehealth in cochlear implant users: From COVID-19 emergency to routine service. Eur Arch Otorhinolaryngol, 280, 5293–5298.
† Remote Check for Nucleus Sound Processors is approved for all ages, however certain tests are not suitable for ages below 6. Remote Check does not replace clinical care and does not involve remote programming of the sound processor. Remote Assist for Nucleus sound processors is approved for ages 6 and older. Remote Check and Remote Assist features are only visible and accessible if they are enabled by a clinician. Clinicians should consider the suitability of the feature before enabling Remote Check and Remote Assist. Only available at clinics that have enrolled in Remote Care. For sound processor and app compatibility information visitwww.cochlear.com/compatibility.
This blog is intended to serve as a resource for clinicians to help keep up to date with current clinical literature and is intended for professionals only. Clinical literature is based on research, which may include the experimental use of new or currently available products and technologies. Therefore, literature presented on this blog may represent use of Cochlear products that does not align with the intended use or indications approved by regulatory bodies, also known as off-label use. Cochlear does not condone any off-label use of its products, and it is not Cochlear’s intent to promote off-label use by providing this blog as a resource for healthcare professionals.


