
In this exclusive interview, we sit down with Dr. Sheryl Lewin, a renowned craniofacial plastic surgeon specializing in pediatric microtia and atresia, to discuss her experience with the Cochlear™ Osia® System†. With over two decades of experience and a practice focused solely on ear reconstruction, Dr. Lewin shares her insights into surgical integration, patient selection, and the transformative impact of the Osia System on pediatric patients.
This conversation is especially relevant for bone conduction surgeons considering the Osia System for patients with conductive hearing loss, mixed hearing loss, or SSD. Dr. Lewin’s experience offers reassurance and practical guidance for integrating the Osia System into complex surgical workflows.
Q: Dr. Lewin, can you share a bit about your background and how you came to specialize in pediatric ear reconstruction?
Dr. Lewin: I actually started in architecture, which gave me a strong foundation in creativity and design. But I found myself wanting a more gratifying career, so I transitioned into medicine and trained at Stanford. Plastic surgery stood out as the most creative and visual specialty, and within that, ear reconstruction is considered one of the most challenging procedures. That challenge drew me in — and now, making ears is all I do.

Q: What makes the Osia System particularly effective for pediatric patients with complex craniofacial anatomy?
Dr. Lewin: The Osia System was a game-changer when it launched in the U.S. in 2020. Unlike previous solutions like the Baha® Attract, the Osia System offers a fully subcutaneous implant with digital piezoelectric stimulation, eliminating external vibration. This is especially beneficial for children with microtia and atresia, where sound processors on softbands often fall short in delivering high-frequency sounds critical for speech development.
For most of my patients, the Osia System is now the go-to solution. We follow standard audiological guidelines for candidacy, focusing on bone conduction thresholds. For younger children or those with thinner skulls, we may delay implantation until their anatomy is more suitable.
Q: How do you integrate Osia System implantation into your surgical planning for ear reconstruction?
Dr. Lewin: Ideally, we perform simultaneous ear reconstruction and Osia System implantation in one surgery. This minimizes anesthesia exposure and gives the child a functional ear immediately. However, in cases with complex anatomy — such as syndromic patients or those with hemifacial microsomia — we often stage the procedures.
For example, in Treacher Collins syndrome, I delay the Osia System until both ears are reconstructed and healthy. This avoids compromising the ear flap and allows for bilateral Osia System placement later. Similarly, in severe hemifacial microsomia, we may need to adjust Osia System placement due to bone irregularities.
Q: What intraoperative techniques have you found helpful in optimizing Osia System outcomes?
Dr. Lewin: One key technique I’ve adopted is placing the superior portion of the OSI300 Implant in a subperiosteal pocket. Pediatric patients often have thin scalp tissue, and the implant coil curvature and rigidity of a magnet-based solution like the Osia System, can cause pressure ulcers. By using the periosteum for coverage, we’ve seen improved tolerance and fewer complications.
I’ve also developed a strict post-op protocol for parents to monitor skin integrity. If redness appears, we pause device use to prevent progression. These steps have been critical in managing potential challenges of these pediatric Osia System cases.
Q: What misconceptions do families have about bone conduction devices, and how do you help them navigate the decision?
Dr. Lewin: Many families don’t understand the difference between the sound processor on a softband and the Osia System. They’re often surprised to learn that the Osia System doesn’t vibrate externally and offers a more stable, discreet solution. I use visuals like the speech banana to show how the Osia System improves access to high-frequency sounds.
We also run an Ear Pals program, where we connect families with other patients who’ve undergone ear reconstruction and Osia System implantation. Hearing directly from older children — especially those who transitioned from soft bands — is incredibly powerful. Their enthusiasm and clarity often resonate more than any clinical explanation.
Q: How do you communicate with pediatric patients and their families in an age-appropriate, reassuring way?
Dr. Lewin: I’m very transparent. I show them the device, explain how the magnet works, and discuss visibility of an implant under the scalp. For kids, I focus on what they’ll be able to hear — like birds chirping or footsteps — and how it will improve their experience at school and in daily life.
I also emphasize that the Osia System isn’t perfect, but it’s a significant upgrade from softbands. Most kids never want to go back once they’ve experienced the Osia System.
Q: Can you share a story where the Osia System significantly improved a child’s confidence or quality of life?
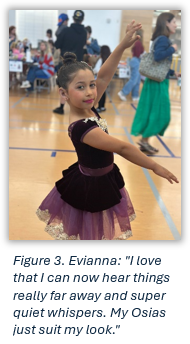
Dr. Lewin: I don’t have just one story — I have hundreds. Families stay in touch for years, sending me videos and updates. One common theme is the delayed realization of benefit. Bilateral patients often feel overstimulated at first, but after a few weeks, they start noticing sounds they’ve never heard before — pages turning, birds, footsteps. Simple things like being able to wear the Osia System in the rain or under a hat help children with hearing loss feel more like their peers.
These moments are incredibly rewarding. They show how the Osia System can transform a child’s auditory world and boost their confidence in ways that go beyond clinical metrics.
Q: What trends have you observed in auditory outcomes or speech development post-Osia System?
Dr. Lewin: While I don’t have direct access to audiological data — many of my patients live out of state — I receive consistent feedback from parents. They report improved speech clarity, better classroom engagement and overall satisfaction. Many parents tell me their kids love their Osia System and wear it full-time.
I’d love to see more collaborative follow-up protocols between surgeons and audiologists to track long-term outcomes more objectively.
Q: What advice would you give to surgeons considering the Osia System for their pediatric patients?
Dr. Lewin: Although Osia System implantation is thought by many to be a simple surgery, for me, I did find there was a learning curve to placing the device in the best position for each patient’s anatomy. Don’t be intimidated by the learning curve. The Osia System offers a unique opportunity to combine functional hearing restoration with aesthetic reconstruction. With proper planning, intraoperative technique and post-op care, outcomes can be excellent — even in complex cases.
Also, engage families early. Transparency, peer support and education go a long way in building trust and ensuring successful adoption.
Dr. Lewin’s experience highlights the versatility and impact of the Osia System in pediatric patients with complex anatomy. Her innovative surgical techniques and patient-centered approach offer a compelling case for expanding Osia System use among bone conduction surgeons.
As more clinicians and surgeons embrace the Osia System, the potential to improve auditory outcomes and quality of life for children with conductive hearing loss, mixed hearing loss, or SSD continues to grow.

Dr. Sheryl Lewin, Porous Implant Ear Reconstruction Surgeon
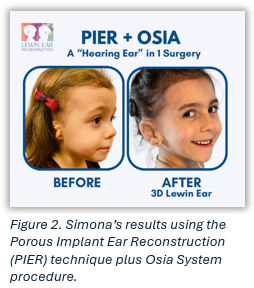
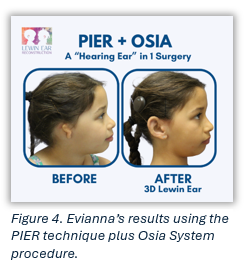
Dr. Lewin is a Craniofacial-trained board-certified Plastic Surgeon. She is one of the leading microtia surgeons of the world treating children and adults with the Porous Implant Ear Reconstruction (“PIER”) technique. She has spent the last 20 years developing innovative techniques to improve the outcome of PIER, including the 3D Lewin Ear Implant by SuPor. Dr. Lewin has implanted approximately 150 Cochlear Osia Hearing Systems to date and can do it during PIER surgery; therefore, the patient gets a “hearing ear” in just one surgery.
Dr. Lewin is the founder of Earicles, Miracles for Ears, a non-profit organization dedicated to help children born with microtia thrive through Education, Advocacy, Research, Surgery (EARS). Find out more here: https://lewinear.com

† In the United States and Canada, the Osia System is cleared for children ages five and older.
Views expressed are those of the individual. Consult your hearing health provider to determine if you are a candidate for Cochlear technology. Outcomes and results may vary.
This blog is intended to serve as a resource for clinicians to help keep up to date with current clinical literature and is intended for professionals only. Clinical literature is based on research, which may include the experimental use of new or currently available products and technologies. Therefore, literature presented on this blog may represent use of Cochlear products that does not align with the intended use or indications approved by regulatory bodies, also known as off-label use. Cochlear does not condone any off-label use of its products, and it is not Cochlear’s intent to promote off-label use by providing this blog as a resource for healthcare professionals.

